Serving as a Certified Nursing Assistant (CNA) in a medical-surgical (med-surg) environment is both emotionally and physically challenging. Navigating the care of patients with a variety of medical needs, enduring long hours, and continuously offering empathy can significantly impact CNAs.
It is crucial for med-surg CNAs to focus on self-care to preserve their health and well-being. This article will delve into the difficulties faced by med-surg nursing assistants and offer actionable self-care advice to assist them in managing the emotional and physical pressures of their role.
What are the responsibilities of a medical-surgical CNA?
A Medical-Surgical Certified Nursing Assistant (Med Surg CNA) is essential in delivering hands-on care to patients within a medical-surgical environment. Their duties encompass helping with everyday activities, tracking vital signs, supporting medical procedures, and providing emotional comfort to both patients and their families. Med Surg CNAs collaborate intimately with medical teams, playing a pivotal role in the care of individuals with various health conditions, thereby enhancing the quality and empathy of healthcare services.
Grasping the emotional challenges
The responsibilities of a med surg CNA involve being at the forefront of patient care, addressing a broad spectrum of medical conditions, and frequently encountering critical situations. Witnessing patients’ distress, interacting with their families, and enduring continuous pressure can result in burnout if not effectively handled.
Furthermore, the physical demands of the job, such as assisting in lifting and relocating patients, can lead to fatigue and musculoskeletal problems.
Techniques for maintaining emotional wellness
- Place emphasis on emotional well-being
- Self-reflection practices: Dedicate time to contemplate challenging situations. Sharing experiences with colleagues or a mentor can offer emotional relief and insights.
- Set clear boundaries: Distinguish between work and personal life. Avoid bringing work stress home and find activities to unwind.
- Cultivate a support network
- Foster connections with peers: Forge strong relationships with colleagues who comprehend the demands of the job, creating a supportive community.
- Seek professional assistance: If the emotional burden becomes overwhelming, consider consulting with a mental health professional specializing in healthcare-related stress.
- Prioritize physical health
- Practice proper body mechanics: Learn and apply correct body mechanics to prevent musculoskeletal injuries. Utilize lifting equipment when available to minimize strain.
- Regular physical activity: Engage in consistent exercise to enhance strength and endurance, serving as a valuable stress reliever.
- Effective time management
- Recognize the importance of breaks: Incorporate regular breaks during shifts to recharge. Even a brief respite can significantly enhance focus and energy levels.
- Efficient scheduling: Organize your schedule efficiently and prioritize tasks to prevent feeling overwhelmed and ensure critical responsibilities are addressed promptly.
- Mindfulness and relaxation techniques
- Deep breathing exercises: Integrate deep breathing exercises into breaks or stressful moments to encourage relaxation.
- Mindfulness practices: Explore mindfulness techniques like meditation or yoga to center your mind and alleviate stress.
- Advocate for yourself and pursue education
- Voice your needs: Communicate your physical and emotional requirements to supervisors, advocating for a supportive work environment promoting employee well-being.
- Lifelong learning: Stay informed about new methods and technologies that can reduce physical strain in your role.
- Make healthy lifestyle choices
- Balanced nutrition: Maintain a well-rounded diet to ensure your body receives essential nutrients, minimizing reliance on caffeine or sugary snacks for energy.
- Sufficient sleep: Prioritize adequate sleep to facilitate recovery for both your body and mind.
Self-care techniques to promote the physical well-being of Medical-Surgical CNAs
The physical aspect of well-being holds significant importance in overall health and can profoundly impact the duties and quality of life for Medical-Surgical CNAs. Incorporating self-care strategies aimed at physical well-being is crucial for sustaining vitality, preventing illness, and fostering longevity.
Below are effective self-care strategies tailored for physical well-being:
- Consistent Exercise: Participate in regular physical activities, encompassing both aerobic exercises like walking, running, or swimming, and strength training. Aim for at least 150 minutes of moderate-intensity exercise per week, aligning with recommendations from health professionals.
- Balanced Nutrition: Maintain a well-rounded diet comprising a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats. Limit the consumption of processed foods, sugar, and excessive caffeine intake.
- Hydration: Ensure adequate hydration by consuming an ample amount of water throughout the day. Water is vital for the body as it assists in digestion, nutrient absorption, and temperature regulation.
- Adequate Sleep: Prioritize obtaining sufficient and quality sleep each night. Aim for 7-9 hours of sleep to facilitate bodily rest, recovery, and overall well-being. Establishing a consistent sleep routine promotes better sleep hygiene.
- Stress Management: Employ stress-reduction techniques such as deep breathing exercises, meditation, or yoga. Chronic stress can adversely affect physical health, underscoring the importance of effective stress management strategies.
- Regular Health Check-ups: Schedule routine check-ups with healthcare providers for preventive care. Consistent screenings, vaccinations, and health assessments aid in early detection of potential issues, facilitating timely intervention.
Achieving a balance between work and personal life for Medical-Surgical CNAs
Attaining a balanced work-life harmony is crucial for overall well-being, entailing a harmonious blend between professional responsibilities and personal pursuits.
Here are key considerations for sustaining a work-life balance as a Medical-Surgical Nursing Assistant:
- Establish clear boundaries between professional and personal time.
- Prioritize self-care by dedicating time for relaxation and recreational activities.
- Learn to delegate tasks and seek assistance when necessary.
- Set achievable goals and avoid overcommitment.
- Utilize technology judiciously to prevent work from intruding into personal time.
- Take regular breaks during the workday to rejuvenate and alleviate stress.
- Maintain open communication with colleagues and supervisors regarding workload and expectations.
- Efficiently plan and organize tasks to enhance productivity.
- Cultivate positive relationships in the workplace and nurture personal connections beyond work.
- Regularly reassess and adapt priorities to sustain a manageable work-life balance.
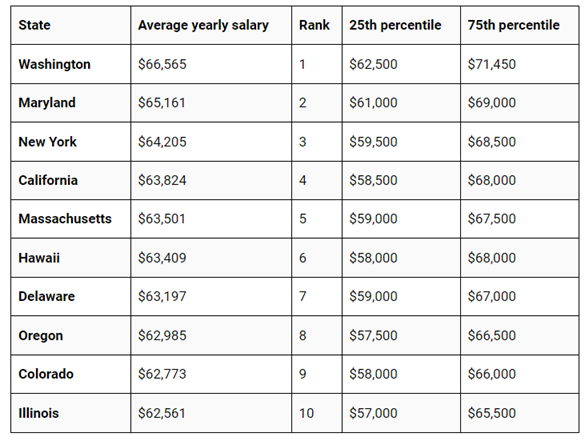
The salary of Medical-Surgical CNAs in the United States
As of January 2024, the average annual salary for Medical-Surgical CNAs in the United States stands at $60,909. Yet, this number may fluctuate considerably due to multiple factors:
- Location: Washington, Maryland, and New York are among the highest-paying states for Med Surg CNAs, whereas Mississippi, Louisiana, and South Dakota are among the lowest-paying states.
- Experience: Typically, CNAs with more experience command higher salaries compared to those with less experience.
- Education: Some CNAs hold a two-year associate’s degree in nursing, while others possess a one-year certificate. Generally, CNAs with higher levels of education tend to earn higher salaries.
- Employer: Compensation can vary based on the type of employer, with hospitals often offering higher salaries compared to nursing homes and other healthcare facilities.
Conclusion
In the challenging realm of medical-surgical care, self-care stands as a vital priority for Certified Nursing Assistants (CNAs). Navigating the emotional and physical strains necessitates the establishment of boundaries, cultivating a supportive network, and placing emphasis on personal well-being.
Incorporating mindfulness, consistent exercise, and efficient time management practices fosters a comprehensive approach to self-care.
Achieving a harmonious work-life balance, making healthy lifestyle decisions, and pursuing ongoing education are crucial components for a rewarding career and securing an effective salary as a med surg CNA.
















